What is Male Infertility, Testing, & Possible Causes (Part 1)
When it comes to Fertility imbalances, many focus on the women’s health, or ability to conceive. There are many products, articles, studies, and opinions on what women should and should not do to realign any infertility conditions. Yet, the information and opinion on Male Infertility falls on deaf ears. Even though, 1 out of 8 couples experience infertility challenges and about 30 to 50 % of the cause of infertility is male factor related. It literally takes two to make a baby. It is always one of our first questions during our Fertility consultations is “Has Male Factor Infertility been ruled out?”, “Has the male partner had a semen analysis, full male hormone, thyroid, and blood panel completed?”
With Conscious Conception, both partners need to prepare their bodies BEFORE trying to conceive for at least 4-6 months. Preparing includes both partners getting blood work completed, semen analysis, possible pelvic ultrasound, an inventory on lifestyle stressors, an assessment of emotional and mental health to take on the fertility journey and intended parenthood, review of current supplements, and adjustment to nutrition.
Here, we will discuss What is Male Infertility, What is Sperm Analysis, The Possible Causes of Infertility, and What are the Western Medicine Ways of Treating Male Infertility?
When considering Male Infertility the following areas need to be reviewed:
Sperm Health and Factors Ruled out by Semen Analysis. “1 in 25 men have sub-fertility that contributes to 50% of infertility causes in couples” (1). The Semen Analysis is usually performed by the fertility clinics. Here, they will take a sample of semen and run several tests to determine the health of the sperm. Each lab will have their own ranges and standards that will be given on the final report, but the WHO, World Health Organization, included some values for Sperm Analysis:
Total count: 39-928 million
Volume: 1.5-7.6 mL
Sperm concentration/count: 15-259 million per mL
Motility (how sperm moves) includes progressive and non-progressive motility: 40-81% moving
Progressive motility (how well moving forward): 32-75% moving
Forms (shape of sperm head and tails): 4-48% (2)
Check into Endocrine Factors (how the hormone systems are balanced) through blood work. It is important to request a CBC with differential, complete male hormone panel, and thyroid panel. For the thyroid panel, make sure the testing includes: TSH, T3, T4, fT3, FT4, TPO, thryoid antibodies, to get a clear picture of thyroid health.
Determine if Lifestyle adjustments Need to be addressed such as certain medications, congenital factors, stress, or possible radiation.
Age Factors: As men get older, the quality of sperm can change. The volume can drop by 20% between the ages of 30 to 50 years old. The count for progressive motile sperm can decrease 5% per year, while motility drops 3% per year (1). Most families start their conception journey by ages 30 to 4o-years-old, so checking in on sperm health will save a lot of headaches.
Possible Causes of Male Infertility:
Testicular disease is a primary cause of male infertility. 66% of the cause is unknown, 20% is due to undescended testes known as Testicular maldescent, or Cryptorchidism, and 7% is due to stagnation from trauma and torsion. The Cryptorchidism is when the testes do not descend into the scrotum. This is usually seen in male infants and toddlers.
Obstructive causes are secondary cause of male infertility, which includes Reversed Vasectomy, Congenital vas deferens absence, and STD scarring. When a man decides to reverse a vasectomy, antibodies can still be present from the procedure and affect male fertility. The congenital vas deferens absence is when the tubes that carry out the sperm out of the testes are missing (3). Sexually Transmitted Disease (STD’s) such as Chlamydia can create scar tissue.
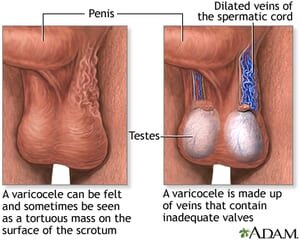
Variocele is when there are dilated veins in the scrotum. This stagnation is usually related to higher anti-sperm antibodies. See image below.
4. Some medications can affect sperm health such as Cytotoxic chemotherapy, Salazopryine, Antiepileptic medication, Testosterone, steroids, and SSRI’s such as Prozac. Steroids are known to decrease sperm count.
5. DNA fragmentation in the sperm head can disrupt the fertilization process where the DNA from the sperm cannot combine to the ovum. This can be assessed by the SCSA, Sperm Chromatin Structure assay.
6. Chemical exposure such as heavy metals, pesticides, and paints can effect our detox pathways, hormonal systems, and reproductive health. There are many ways to test and treat these chemical exposures.
7. Stress leaves us in either a fight, flight, freeze, or fawning mode. It is difficult for the brain to calm and let go. Under constant, high stress, the body will focus on survival, so all circulation will go to the limbs to respond to the perceived threat instead to the reproductive organs.
8. Radiation & Constriction: Did you know 30% decrease in sperm count and motility happens after leaving a cell phone in the front pocket for 4 hours? The cell phone creates radiation and heat which can fry sperm. The reason why the testes and scrotum hang lower and outside of the pelvis is to keep cooler than the average body temperature of 98.6 degree F. The tight jeans need to be switched out to boxer shorts because any tightness can create constriction.
9. Anti-sperm Antibodies are immune factors in males that effects male fertility. The anti-sperm antibodies can be seen in vasectomy reversal, prostatitis, and inguinal hernia. 9-36% of infertile men will have the anti-sperm antibodies, while 70% of men with this came from reproductive surgeries. In Western Medicine, this would be treated with immunosuppressive medication such as corticosteroids, or cyclosprone, alongside ART, IVF, IUI, and/or sperm injection. The sperm would go through a sperm washing to wash off the anti-sperm antibodies. With this method, IVF is not affected by the anti-sperm antibodies. The challenge with this treatment is the procedures are invasive, have possible side effects from the medication, and lower efficacy.
Western Medicine Approach to Male Infertility usually includes IVF, In-vitro Fertilization, IUI, Intrauterine Insemination, or ICSI, Intracytoplasmic sperm injection. Sometimes other medications and synthetic medications will be used for both the man and woman to help control the cycle, ovulation, and sperm health. The sperm washing will be used to wash of anti-sperm antibody. Some Fertility Specialists will recommend some lifestyle adjustments such as nutrition, supplementation, stress-management, and possible Acupuncture. We will discuss how Sperm Health can be improved with Acupuncture, Herbal Medicine, Supplements, and Nutrition in Part 2 blog.
References:
“Male Fertility: Treatment of Infertility by Jane Lyttleton, L.Ac., CEU Class
WHO Sperm Analysis Stats: https://www.healthline.com/health/mens-health/normal-sperm-count
“Congenital bilateral absence of the vas deferens” . U.S. National Library of Medicine 8600 Rockville Pike, Bethesda, MD 20894 U.S. Department of Health and Human Services National Institutes of Health. 18 August 2020. https://medlineplus.gov/genetics/condition/congenital-bilateral-absence-of-the-vas-deferens/